- Home
- About Us
- Membership
- Partners
- Resources
- Education & Events
- Advocacy
- Advocacy Letters
- COVID-19
- Shared Savings Program
- Medicaid ACOs
- CMMI Models
- ACO Program Elements
- Quality and Equity
- Congress
- Payment Rules
- Other Regulations
- News
- ACO News
- NAACOS Blog
- NAACOS In the News
- NAACOS Member News
- Press Releases & Letters
|
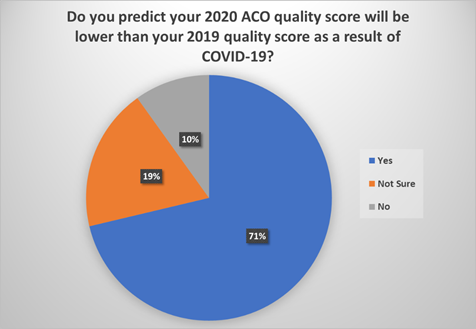
February 10, 2021 Liz Richter Re: Request to Change Medicare Shared Savings Program Quality Reporting Scoring for Performance Year 2020 Due to COVID-19 Dear Acting Administrator Richter: The National Association of ACOs (NAACOS) appreciates the opportunity to provide recent feedback from Accountable Care Organizations (ACOs) in the Medicare Shared Savings Program (MSSP) about concerns related to 2020 quality reporting, which has been negatively affected by the COVID-19 pandemic. NAACOS shares this feedback along with a request for the Centers for Medicare & Medicaid Services (CMS) to change the agency’s policy to provide MSSP ACOs with their 2020 quality score for performance year (PY) or the average MSSP quality score, due to the impact of COVID-19. This policy was included in the Final 2021 Medicare Physician Fee Schedule Rule (CMS-1734-P), as published in the Federal Register on December 28, 2020. This was a departure from the alternative policy put forward by the agency in the proposed rule, which was strongly supported by NAACOS and many stakeholders. NAACOS is the largest association of ACOs, representing more than 7 million beneficiary lives through more than 370 MSSP, Next Generation (Next Gen) ACO Model, and commercial ACOs. NAACOS is an ACO member-led and member-owned nonprofit that works on behalf of ACOs across the nation to improve the quality of care delivery, population health, patient outcomes, and healthcare cost efficiency. Quality improvement is a cornerstone of the ACO model. In addition to reducing spending, ACOs must meet certain quality performance standards to be eligible to receive shared savings payments. ACOs continue to improve quality year over year, which improves patient care and helps to control costs. It is critical that CMS policies to evaluate ACO quality are fair, appropriate, and accurately reflect the work ACOs engage in to improve patient care. Effects of COVID-19 on ACOs NAACOS has greatly appreciated numerous CMS actions and policy changes to protect ACOs and other APM participants in the face of the pandemic. For example, we supported a number of changes the agency enacted to protect ACOs from harmful effects of COVID-19, such as allowing MSSP ACOs to extend agreements for an additional year through 2020, removing the requirement for ACOs to field a Consumer Assessment of Healthcare Providers and Systems (CAHPS) for ACOs Survey for PY 2020, pausing the MSSP risk glide path for 2021, extending the Next Generation ACO Model through 2021, removing expenditures for patients with COVID-19, expanding use of telehealth, and more. Implementing these policy changes strengthens the long-term value movement, therefore enabling ACOs to be part of the solution when recovering from this pandemic and beyond. Request for CMS to provide MSSP ACOs with the higher of their 2019 or 2020 quality scores Unfortunately, CMS decided to maintain its extreme and uncontrollable circumstances policy. Therefore, ACOs will receive the higher of their own 2020 quality score or the mean 2020 MSSP ACO quality score if they are unable to report quality data due to the COVID-19 PHE. NAACOS and the ACO community are disappointed with this policy, which is not appropriate in the face of the pandemic. Many ACOs will have lower quality scores for 2020 due to avoidance of care, resulting in a lower MSSP mean, which would therefore lower shared savings payments at a time when many healthcare providers are also facing other financial challenges. We request that the administration support hard working, financially stressed health workers and ACOs during this difficult time by enhancing opportunities for shared savings, not diminishing them. Specifically, NAACOS requests swift action to instead provide ACOs with the higher of their 2019 or 2020 quality scores. It’s important to note that for the Next Gen Model, CMS is doing just that and will provide the higher of the Next Gen ACO’s 2019 or 2020 quality score due to the impact of COVID-19 on quality improvement efforts. ACOs are concerned about the effect of COVID-19 on ACO quality
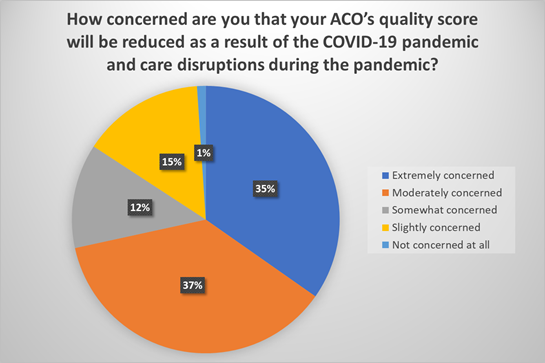
When drilling down further, 99 percent of respondents reported they are concerned that their quality score will be reduced due to the pandemic. The two most popular answers, “extremely concerned” and “moderately concerned” represent 72 percent of responses. Many have predicted that quality scores will be lower in 2020 than in previous years as a result of care disruptions and patients delaying routine preventive care and screenings as a result of the pandemic. The answers to this question further illustrate the concern among ACOs.
Finally, when asked if ACOs think their shared savings will be reduced as a result of their ACOs’ quality score in 2020, almost half (46 percent) reported they expect that will be the case, while 38 percent reported they are unsure, and the remainder said no. These concerns and uncertainty among ACOs come at a time when they are focused on combating the pandemic on the front lines of healthcare. Many staff who would typically be responsible for quality assessments and reporting have been diverted to clinical care, answering patient calls about the pandemic, and efforts to educate and provide vaccines. Providing those critical services means ACOs have fewer resources to report quality, and those who can’t report will likely see their quality scores fall from 2019 as a result of the MSSP policy. Additionally, those ACOs who provide high quality care may still see significant drops in scores due to patients avoiding routine and preventive care during the pandemic, while ACOs are still being held to benchmark performance from pre-pandemic years. Conclusion Sincerely,
Clif Gaus, Sc.D. |