Analysis of ACO Provider-Level (TIN/NPI) QP StatusObjective: Calculate 2021 QP scores at the provider level for TINs or NPIs participating in a given ACOs. Data and Methods: We calculate the QP scores and component numerator and denominator values for each of three QP measurement periods (snapshots) in 2019. For denominators, we identify attribution eligible beneficiaries treated by each ACO using the methodology provided in CMS documentation describing the calculation of QP values at the ACO level. To calculate numerators for Medicaid Shared Savings Program (MSSP) ACOs we use attributed beneficiaries from Q3 2019 provisional attribution lists provided by CMS. We then calculate QP values based on both the patient count and Part B payments methods at both the ACO and TIN levels. For MSSP ACOs, we will provide both denominators (total FFS spending) and numerators (ACO attributed beneficiary spending) and QP scores by TIN. For NextGen ACOs (NGACOs) we will calculate QP denominators for each NPI. CMS does not provide NGACO beneficiary attribution lists, but we can work with individual ACOs to simulate NGACO attribution. (See Appendix for definitions and more detail on methods). The quarterly data has final adjudicated claims with a 3-month runout period; CMS does not refresh the data over time. This results in slight difference in the results we generate compared with what CMS ultimately provides. Our analysis is solely based on MSSP or NGACO participation and it does not account for other advanced APMs or non-Medicare APMs. What we need from you: For MSSP ACOs we will need a provider list that includes TINs, with associated NPIs, and CCNs for RHC, FQHCs and CAHs. This must include the Legal Business Name (LBN) for each TIN. For NGACOs we need the information described above except that we do not require TIN information. These lists need to be provided in excel, CSV, or SAS dataset format. If available, we also request that you provide the most recent QP scores that you have received from CMS to assist us with benchmarking results. What we will do: We will take your ACO’s provider lists and use Medicare carrier and outpatient claims and Medicare enrollment data to calculate QP scores at ACO, TIN and NPI levels. If you are an MSSP ACO, we will use beneficiary attribution provided by CMS. For NGACOs we would need to run attribution to determine the QP status numerators which will require additional time and resources. We will also need to run attribution for certain MSSP ACOs including new ACOs starting after July 1, 2019 or new TIN configurations. What you get: Once done we will provide a report in Excel that includes both ACO and TIN level QP patient and payment threshold scores for each snapshot period. NPI level reports can also be created, but results may be more variable due to the smaller unit size; results for providers with few Medicare patients will be redacted by CMS. This report will include a “Marginal QP Contribution” score for each TIN to help assess the level of contribution of each TIN to the ACO’s overall QP score. We can also estimate QP scores for specific TIN configuration scenarios you are considering that include TINs that are not currently part of your ACO. These scenarios require that we recalculate attribution for the specific providers in each scenario. We provide a separate report for each scenario that is requested. We can run scenarios for any set of TINs or NPIs that you wish to look at. The cost of modeling scenarios is based on the number of scenarios requested. Once the report is delivered, we will set up a call to walk through the report and answer questions. NGACO QP Calculation: We are currently refining our NGACO beneficiary attribution algorithm and cannot guarantee a timeframe for calculating NGACO numerator values. We are willing to work with NGACOs to refine and test our attribution model in order to accurately calculate QP numerators and QP scores. Timeline: Timing will depend on the nature of each request and the volume of requests that we receive but can generally be completed within two weeks. Requests will be taken on a first-come, first-served basis. We will work with each requesting entity to establish a timeline. Rush orders are possible for an additional fee. Contacts: Appendix: Definitions and Methods Attribution eligible beneficiaries for the denominator: We follow the CMS guidelines. Specifically, a beneficiary must:
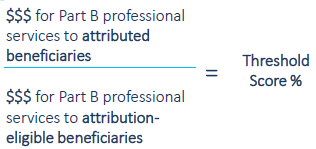
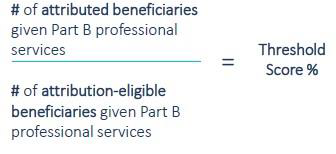
Numerator: This is defined by Medicare beneficiaries attributed to the MSSP or NextGen ACO following the rules for the specific model. QP Status: CMS describes the following definitions for the QP status threshold scores. For payment amount method: For beneficiary count method: Marginal QP Status: CMS calculate QP scores at the ACO level. We mimicked this approach and used the ACO’s provider list to identify the Medicare beneficiaries receiving services at each ACO TIN and used these claims to calculate TIN QP scores. Specifically:
Snap Shots:
|