- Home
- About Us
- Membership
- Partners
- Resources
- Education & Events
- Advocacy
- Advocacy Letters
- COVID-19
- Shared Savings Program
- Medicaid ACOs
- CMMI Models
- ACO Program Elements
- Quality and Equity
- Congress
- Payment Rules
- Other Regulations
- News
- ACO News
- NAACOS Blog
- NAACOS In the News
- NAACOS Member News
- Press Releases & Letters
ACO Survey Shows Why Congress Should Address Value-based Payment Incentives
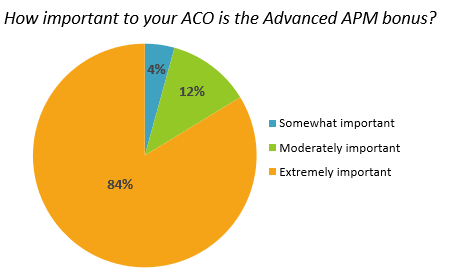
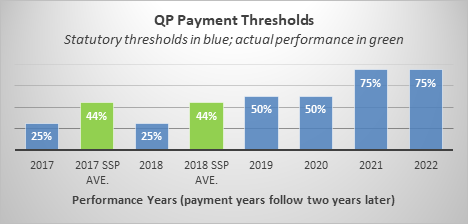
Background: A 2015 law passed by Congress sought to put Medicare on a financially sustainable path by incentivizing participation in alternative payment models (APMs), which are designed to make doctors and hospitals financially accountable for lowering patients' medical spending and improving quality. That law, the Medicare Access and CHIP Reauthorization Act (MACRA), provides bonuses for participating in risk-bearing Advanced APMs, which include accountable care organizations (ACOs). To earn the bonus, clinicians must meet Qualifying APM Participant (QP) thresholds, which are based on the proportion of payments made under, or patients in, the APM. While the bonuses have been a meaningful incentive, the law increases these thresholds to an unreasonable level starting in 2021, and many doctors, hospitals and ACOs that would qualify under this year’s standard will be ineligible. It’s important to note that ACOs currently comprise the vast majority of those earning Advance APM bonuses. Survey Overview: In early September, the National Association of ACOs (NAACOS) emailed all ACOs participating in Advanced APMs, which includes the Medicare Shared Savings Program’s (MSSP’s) Track 1+, Track 2, Basic Level E, Enhanced Track, and the Next Generation ACO Model. The online survey was sent to NAACOS members and non-members, with a request for feedback on the Advanced APM bonus and QP thresholds. There were 216 responses from 116 ACOs across the country. Key Takeaways: The survey results send a clear and strong message that the Advanced APM bonus has meaningfully supported ACOs moving to risk-based models and has funded patient-focused initiatives such as care coordination efforts. However, in response to rising QP thresholds, ACOs are very concerned they will no longer receive the bonus, which could threaten Medicare’s move to value-based payment. While many ACOs cited attempts to increase their QP scores through efforts such as increased patient outreach, more than 90 percent of ACO respondents reported they are concerned they will not meet the QP thresholds in 2021. There is good reason for their concern, according to the QP scores reported by respondents for the first quarter of 2020, 96 percent would fall short of the 2021 QP payment amount threshold. To fix this problem and maintain this important incentive for ACOs and other Advanced APM participants, Congress should take swift action to address QP thresholds. Detailed Survey Findings The Advanced APM bonus has been very meaningful to ACOs and has advanced the shift to value.
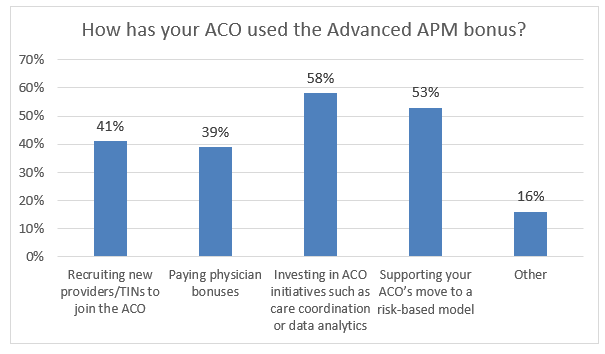
When asked how their ACO has used the Advanced APM bonus, the most popular answers were investing in ACO initiatives such as care coordination and data analytics and supporting their ACO’s move to a risk-based model. These responses show the beneficial ways these funds have been used.
It is already very challenging to meet existing QP thresholds.
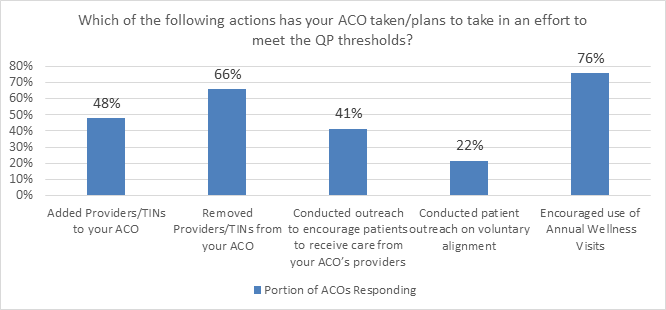
When asked how easy or difficult it is to meet the current QP thresholds, more ACO respondents (42 percent) reported that it was difficult or very difficult compared to 28 percent of survey respondents reporting that it was easy to meet the current thresholds. While it is difficult to meaningfully increase QP scores, ACOs have attempted to do so and shared those strategies in this survey. Specifically, as shown below, the survey reveals that the most prevalent efforts among survey respondents to increase QP scores are by increasing engagement with beneficiaries, through outreach and encouraging patients to see ACO providers or have annual wellness visits, or by removing certain providers from the ACO. The latter is concerning because dropping providers means less engagement in a value-based model and fewer benefits for patients. This unfortunate unintended consequence of challenging QP thresholds typically results in ACOs removing more specialty focused providers compared to primary care providers, thus limiting the overall shift to value.
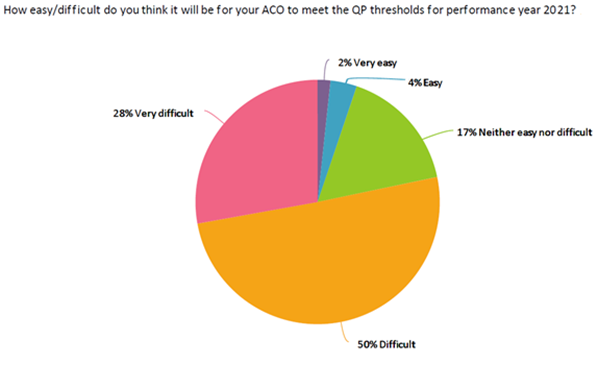
Despite efforts to increase QP scores, the PY 2021 thresholds are far too high.
Conclusion and Solution To fix this problem, Congress should update QP thresholds so they do not rise above 50 percent in 2021 to ensure providers can still qualify for value-based payment incentives. Additionally, Congress should permit the Secretary to raise the QP thresholds by no more than 5 percent per year to minimize provider burden. For performance years affected by the COVID-19 Public Health Emergency, Congress should permit the Department of Health and Human Services to disregard the QP thresholds and award the Advanced APM bonus to providers participating in qualifying models. [1] Page 50384 of the proposed 2021 Medicare Physician Fee Schedule rule, published in the Federal Register August 17, 2020, estimates between 196,000 and 252,000 QPs for Performance Year (PY) 2021, which is fewer QPs than in PY 2019 or PY 2020. [2] The 2018 Quality Payment Program Experience Report is available on this CMS webpage. |