|
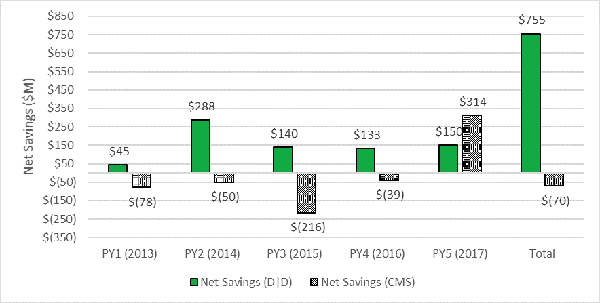
News Release New Independent Analysis Shows ACOs Have Saved Medicare $3.53 Billion WASHINGTON – In the third iteration of the work, an independent evaluation found accountable care organizations (ACOs), Medicare’s dominant value-based care initiative serving nearly 11 million seniors, lowered spending by $3.53 billion from 2013 to 2017 and saved $755 million after paying shared savings. Results show the Medicare Shared Savings Program’s benefits continue to grow and are greater than other sources have credited the program. The Centers for Medicare & Medicaid Services (CMS) has judged performance based on benchmarks, an ACO’s annual, pre-determined spending target. This new, independent evaluation, conducted by the analytic firm Dobson | DaVanzo & Associates, compared ACO spending to similar non-ACO providers and patients to determine what spending would be in the absence of ACOs. The firm used research methods called as-treated difference-in-differences design, which are rigorous and widely accepted to estimate savings and losses. Dobson previously conducted analysis through 2015 and 2016. The Medicare Payment Advisory Commission (MedPAC) has used a similar approach to analyze ACO savings. See the Full Report. “These results are undeniable,” said Clif Gaus, Sc.D., President and CEO of the National Association of ACOs (NAACOS). “There hasn’t been another voluntary initiative in Medicare that has generated billions in savings over such a short period of time.” Medicare Shared Savings Program Savings for 2013–2017 after Accounting for Shared Savings Payments
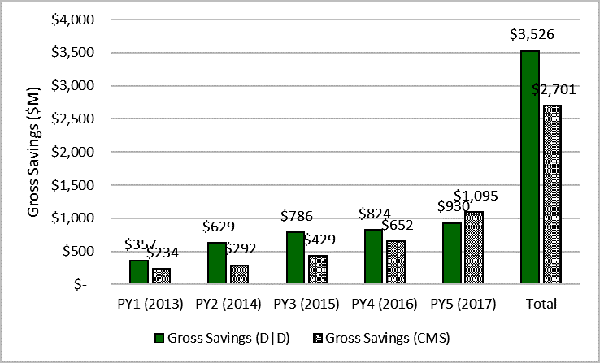
"Time and time again, ACOs have proven superior to Medicare’s other value-based care initiatives. CMS and Congress should look for ways to bolster ACO participation to further drive these savings," Gaus said. The latest research found the Shared Savings Program generated around 1 percent in savings relative to comparison groups, which is consistent with what others, including MedPAC in its June 2019 report to Congress, have reported. Distinguished researchers from Harvard University have also shown similar results. ACOs in the Shared Savings Program care for nearly 11 million Medicare seniors through 518 ACOs, although the latter number is down from 561 ACOs last year after changes CMS enacted through its Pathways to Success regulation. Gross Savings in the Medicare Shared Savings Program for 2013–2016
The ACO model is a market-based solution to fragmented and costly care that empowers local physicians, hospitals, and other providers to work together and take responsibility for improving quality, lowering spending, and providing better outcomes. Providers can earn back part of the savings they generate for Medicare by hitting pre-determined spending goals. Importantly, the ACO model also maintains patient choice of clinicians and other providers. Origins of Medicare ACOs date back to the George W. Bush administration, and ACOs have been instrumental in the bipartisan goal to shift the health system to value-based care. A central part of the ACO concept is to transform health care through meaningful clinical and operational changes to put patients first by improving their care and reducing unnecessary expenditures. Contact: |