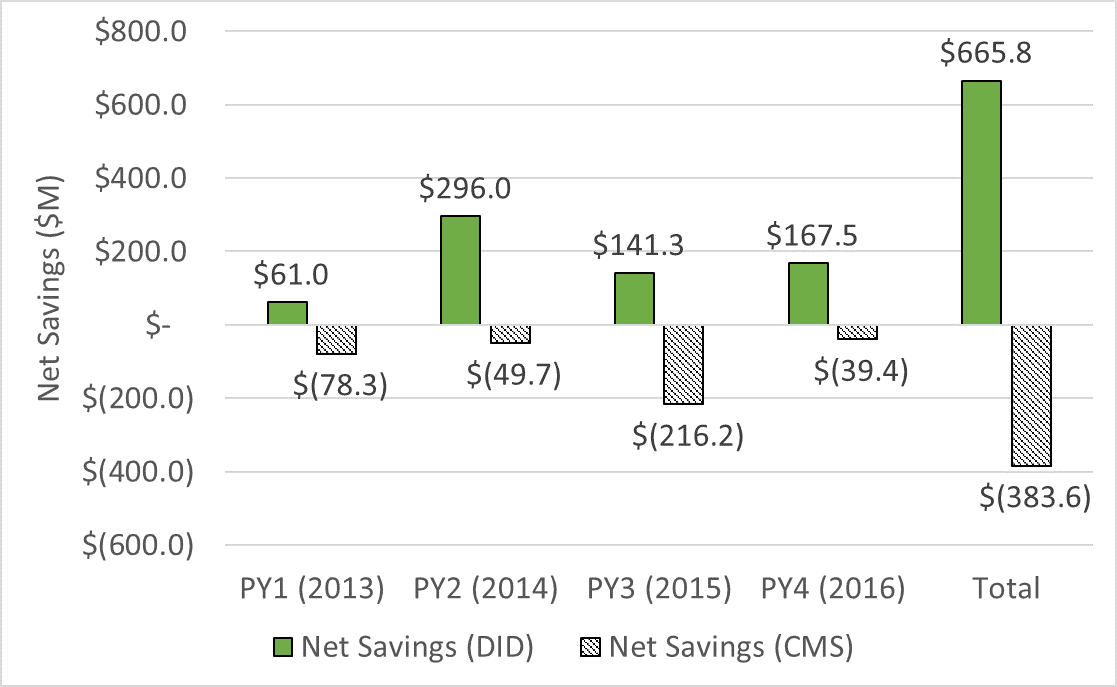
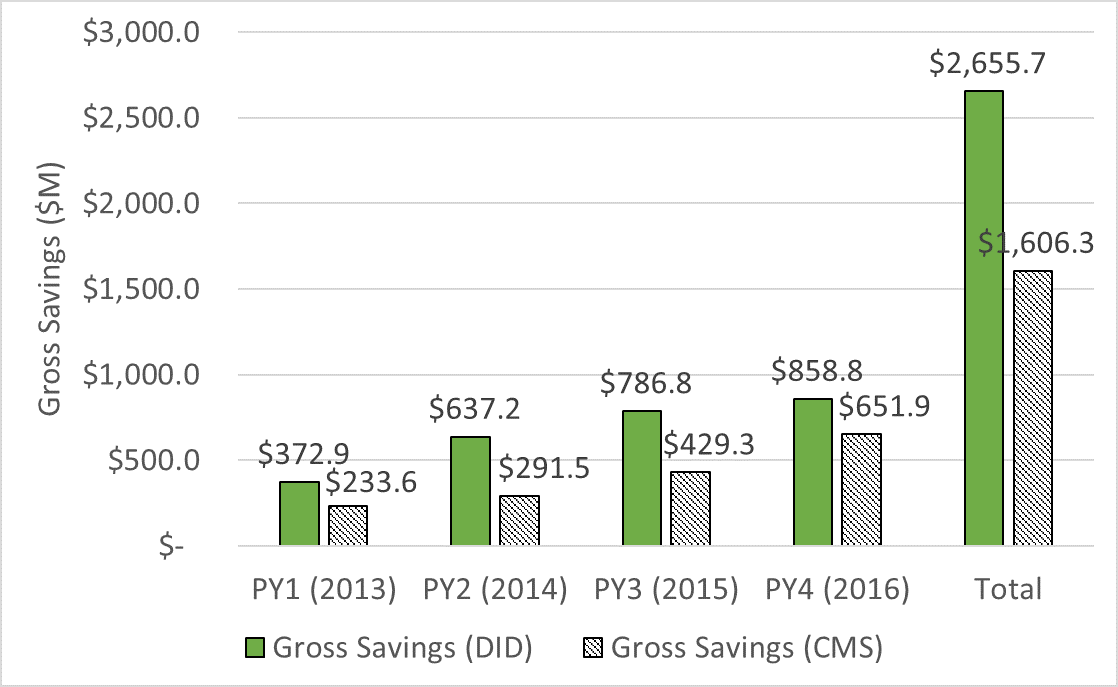
ACOs Saved Medicare $2.7 Billion to DateMedicare Trust Fund Netted More than $660 Million from 2013–2016 WASHINGTON —In the latest data proving the financial benefits of accountable care organizations (ACOs), Medicare’s largest value-based care initiative – the Medicare Shared Savings Program – saved $859 million in 2016, an independent analysis published today shows. Since 2013, the first full year of the program, ACOs have saved Medicare $2.66 billion, well above the $1.6 billion calculated by the Centers for Medicare and Medicaid Services (CMS). After accounting for bonuses paid to ACOs for hitting spending and quality targets, the program, which accounts for 561 ACOs and 10.5 million patients nationwide, netted more than $660 million to the Medicare Trust Fund between 2013 and 2016, contrasting the net loss of $384 million CMS estimates. See the Full Report “These results are the latest data point in a growing body of evidence unequivocally proving ACOs’ value,” said Clif Gaus, Sc.D., president and CEO of the National Association of ACOs (NAACOS). “ACOs are saving American taxpayers hundreds of millions of dollars at a time when it’s most needed.” Medicare Shared Savings Program for 2013–2016 after Accounting for Shared Savings Payments
Source: Dobson | DaVanzo analysis of ACO RIF Data, CMS DUA 28643 and CMS MSSP Public Use Files, 2013-2016 This independent evaluation, conducted by the analytic firm Dobson | DaVanzo & Associates, compared ACO spending to similar non-ACO providers to determine what spending would be like in the absence of ACOs. The firm used research methods that are rigorous and widely accepted to estimate savings and losses. The Medicare Payment Advisory Commission has said it’s conducting its own analysis using a similar approach. CMS has judged performance based on benchmarks, an ACO’s annual, pre-determined spending target, which underestimates performance. Today’s work is a continuation of an analysis NAACOS released in September that examined Shared Savings ACOs, which saved $1.8 billion from 2013 through 2015 and reduced Medicare spending by $542 million. Gross Savings in the Medicare Shared Savings Program for 2013–2016
Source: Dobson | DaVanzo analysis of ACO RIF Data, CMS DUA 28643 and CMS MSSP Public Use Files, 2013-2016 The ACO model is a market-based solution to fragmented and costly care that empowers local physicians, hospitals, and other providers to work together and take responsibility for improving quality, enhancing patient experience, and reducing waste. Providers can earn back part of the savings they generate for Medicare by hitting pre-determined spending goals. Importantly, the ACO model also maintains patient choice of clinicians and other providers. Origins of Medicare ACOs date back to the George W. Bush administration, and ACOs have been instrumental in the bipartisan goal to shift the health system to value-based care. A central part of the ACO concept is to transform health care through meaningful clinical and operational changes to put patients first by improving their care and reducing unnecessary expenditures. “Given the natural lag time in collecting and analyzing data and the well-established trend that ACOs need a few years to start demonstrating results, we are only seeing the beginning of the nation’s return on investment in accountable care,” Gaus said. “This data doesn’t even mention the quality benefits ACOs have generated, which have also been substantial.” A sizable amount of recent data show ACOs are saving money: 472 Shared Savings ACOs generated gross savings of $1.1 billion and netted $314 million in savings to the Medicare Trust Fund last year; CMS’s August 17 proposed rule estimates the overall impact of ACOs, including “spillover effects” on Medicare spending outside of the ACO program, lowered spending by $1.8–$4.2 billion in 2016 alone. Savings have also been calculated by the Health and Human Services Inspector General and researchers at Harvard University. |