Download as PDF
| About the Award
The NAACOS Leaders in Quality Excellence Awards recognize ACOs working to improve the quality and safety of patient care and advance population health goals. From the field of ACOs submitting projects, the NAACOS Quality Committee selected the top three to showcase the quality improvement efforts undertaken by NAACOS members and to disseminate best practices. The three inaugural winners—Essentia Health, Ochsner Accountable Care Network, and Primaria ACO—exemplify how ACOs across the country are improving care by addressing food insecurity, making house calls to reduce preventable emergency department (ED) visits, and engaging patients in preventive services.
The following criteria were used to select the winners:
- Innovation – in processes or technology used to improve performance.
- Improvement – in quality as a result of the intervention or innovative strategies used.
- Scalability and long-term contributions – how can the project’s work be continued, is it scalable, sustainable, transferrable and what was the return on investment.
|
|
2021 NAACOS Leaders in Quality Excellence Award Winners
Essentia Uses High-Tech, High-Touch Outreach to Meet Social Needs
Serving people across rural Minnesota, Wisconsin, and North Dakota, Essentia recognized that food insecurity was a major problem and putting the ACO’s patients at higher risk for chronic conditions like diabetes and heart disease. To tackle the issue, Essentia piloted a screening program at three clinics to identify social needs, including food insecurity, transportation issues, and financial strain. Before every visit, patients are asked to complete a questionnaire available through the ACO’s electronic health record (EHR) patient portal. Essentia also developed an
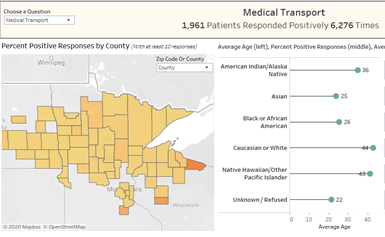 interactive dashboard to map social needs across the ACO’s service area and track performance metrics. When the COVID-19 pandemic hit the region in April 2020, Essentia rapidly scaled the initiative to more than 70 clinics. Since then, more than 420,000 patients have completed the screening questionnaire. Patients who report a social need are then asked if they would like to be contacted by a community health worker to help connect them to community-based resources. interactive dashboard to map social needs across the ACO’s service area and track performance metrics. When the COVID-19 pandemic hit the region in April 2020, Essentia rapidly scaled the initiative to more than 70 clinics. Since then, more than 420,000 patients have completed the screening questionnaire. Patients who report a social need are then asked if they would like to be contacted by a community health worker to help connect them to community-based resources.
About 13.5 percent of patients reported at least one social need, but the screening results show social needs are distributed unevenly across the population. For example, 22 percent of American Indian/Alaskan Native patients and 17 percent of Black patients reported food insecurity  compared to 7 percent of white patients. The ACO also conducted outreach to patients with underlying chronic conditions that put them at high risk for severe COVID illness to make sure they could stay home safely. Essentia has built referral relationships with more than 80 community-based organizations and plans to use Aunt Bertha, an electronic referral platform that connects people to community resources, to build a more sustainable social care network. At the same time, Essentia plans to start deeper compared to 7 percent of white patients. The ACO also conducted outreach to patients with underlying chronic conditions that put them at high risk for severe COVID illness to make sure they could stay home safely. Essentia has built referral relationships with more than 80 community-based organizations and plans to use Aunt Bertha, an electronic referral platform that connects people to community resources, to build a more sustainable social care network. At the same time, Essentia plans to start deeper
|
|
|
level work to consider the broader context around poverty and inequity in the ACO’s communities.
Ochsner Offers On-Demand Home Visits Designed to Reduce Preventable ED Visits
Partnering with Ready, a telehealth firm that dispatches health care professionals to patients’ homes, the New Orleans-based Ochsner Accountable Care Network was able to reduce preventable ED visits by almost 50 percent for more than 500 high-risk Medicaid and Medicare patients. The initiative takes a three-prong approach. 
The Ready at Discharge program, designed to bridge care until newly discharged patients can follow up with their primary care clinician, dispatches an EMT, paramedic or registered nurse to the patient’s home to review symptoms and provide minor treatments and services such as COVID tests. During the visit, the Ready responder and patient consult with the prescribing clinician to review and address any patient concerns.
Ready Community Care takes a similar approach but with a different group of patients—those who frequently visit the ED and/or have multiple non-acute inpatient stays. The Ready responder makes three to five home visits a month for up to three months to take a deep dive into identifying what matters most to the patient and addressing underlying social needs that can contribute to high ED and hospital utilization. Along with establishing a strong link to primary care, the Ready responder connects patients to community resources and provides coaching to help improve health choices. For a select group of high-risk patients, the House Call program essentially provides mobile urgent care on demand. Launched to help connect patients to care for non-emergency health issues that could escalate if left unaddressed, the House Call program sends a Ready responder to the patient’s location to take vital signs and conduct an initial assessment. Following the assessment, the responder on site uses an iPad to initiate a video consult with a licensed physician or nurse practitioner who diagnoses the patient and develops a treatment plan, which might include a prescription or referral to another care setting.
Primaria ACO Forms Quality Team to Close Gaps in Care
In 2017, less than a third of the Indiana-based ACO’s patients were receiving recommended colorectal cancer screenings and less than half were getting screened for breast cancer. Designed to close these gaps in care, the  ACO launched a Quality Team to educate patients about the importance of regular visits with their primary care clinician and completing indicated health screenings. They call patients to let them know they are overdue for a visit or screening and help them schedule appointments. The ACO also identifies higher risk patients who could benefit from more individualized care by using “Best Practice Alerts” to make sure clinicians are aware of specific concerns or patient issues. For example, patients with diabetes who have an A1c score over 9 are flagged, and the Quality Team engages the patients and helps them schedule an appointment with a pharmacist as needed. Between 2017 and 209, the ACO’s percentage of diabetic patients with poor A1c control dropped from 14 percent to 7.6 percent. Primaria also focuses on improving communication and collaboration among clinicians, including primary care clinicians, specialists, case managers, social workers, and other team members. For example, physicians who identify a patient with a social need, such as transportation to an appointment, can contact a resource coordinator to work with the patient and arrange transportation. With the pandemic stalling many preventive health screenings, the Primaria Quality Team is redoubling efforts to notify patients who are overdue for preventive care. If patients are unable to make an in-person visit for certain screenings, the ACO sends an at-home screening kit. ACO launched a Quality Team to educate patients about the importance of regular visits with their primary care clinician and completing indicated health screenings. They call patients to let them know they are overdue for a visit or screening and help them schedule appointments. The ACO also identifies higher risk patients who could benefit from more individualized care by using “Best Practice Alerts” to make sure clinicians are aware of specific concerns or patient issues. For example, patients with diabetes who have an A1c score over 9 are flagged, and the Quality Team engages the patients and helps them schedule an appointment with a pharmacist as needed. Between 2017 and 209, the ACO’s percentage of diabetic patients with poor A1c control dropped from 14 percent to 7.6 percent. Primaria also focuses on improving communication and collaboration among clinicians, including primary care clinicians, specialists, case managers, social workers, and other team members. For example, physicians who identify a patient with a social need, such as transportation to an appointment, can contact a resource coordinator to work with the patient and arrange transportation. With the pandemic stalling many preventive health screenings, the Primaria Quality Team is redoubling efforts to notify patients who are overdue for preventive care. If patients are unable to make an in-person visit for certain screenings, the ACO sends an at-home screening kit.
|
|

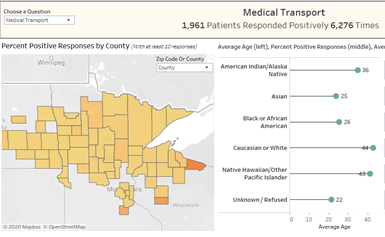 interactive dashboard to map social needs across the ACO’s service area and track performance metrics. When the COVID-19 pandemic hit the region in April 2020, Essentia rapidly scaled the initiative to more than 70 clinics. Since then, more than 420,000 patients have completed the screening questionnaire. Patients who report a social need are then asked if they would like to be contacted by a community health worker to help connect them to community-based resources.
interactive dashboard to map social needs across the ACO’s service area and track performance metrics. When the COVID-19 pandemic hit the region in April 2020, Essentia rapidly scaled the initiative to more than 70 clinics. Since then, more than 420,000 patients have completed the screening questionnaire. Patients who report a social need are then asked if they would like to be contacted by a community health worker to help connect them to community-based resources. compared to 7 percent of white patients. The ACO also conducted outreach to patients with underlying chronic conditions that put them at high risk for severe COVID illness to make sure they could stay home safely. Essentia has built referral relationships with more than 80 community-based organizations and plans to use Aunt Bertha, an electronic referral platform that connects people to community
compared to 7 percent of white patients. The ACO also conducted outreach to patients with underlying chronic conditions that put them at high risk for severe COVID illness to make sure they could stay home safely. Essentia has built referral relationships with more than 80 community-based organizations and plans to use Aunt Bertha, an electronic referral platform that connects people to community 
 ACO launched a Quality Team to educate patients about the importance of regular visits with their primary care clinician and completing indicated health screenings. They call patients to let them know they are overdue for a visit or screening and help them schedule appointments. The ACO also identifies higher risk patients who could benefit from more individualized care by using “Best Practice Alerts” to make sure clinicians are aware of specific concerns or patient issues. For example, patients with diabetes who have an A1c score over 9 are flagged, and the Quality Team engages the patients and helps them schedule an appointment with a pharmacist as needed. Between 2017 and 209, the ACO’s percentage of diabetic patients with poor A1c control dropped from 14 percent to 7.6 percent. Primaria also focuses on improving communication and collaboration among clinicians, including primary care clinicians, specialists, case managers, social workers, and other team members. For example, physicians who identify a patient with a social need, such as transportation to an appointment, can contact a resource coordinator to work with the patient and arrange transportation. With the pandemic stalling many preventive health screenings, the Primaria Quality Team is redoubling efforts to notify patients who are overdue for preventive care. If patients are unable to make an in-person visit for certain screenings, the ACO sends an at-home screening kit.
ACO launched a Quality Team to educate patients about the importance of regular visits with their primary care clinician and completing indicated health screenings. They call patients to let them know they are overdue for a visit or screening and help them schedule appointments. The ACO also identifies higher risk patients who could benefit from more individualized care by using “Best Practice Alerts” to make sure clinicians are aware of specific concerns or patient issues. For example, patients with diabetes who have an A1c score over 9 are flagged, and the Quality Team engages the patients and helps them schedule an appointment with a pharmacist as needed. Between 2017 and 209, the ACO’s percentage of diabetic patients with poor A1c control dropped from 14 percent to 7.6 percent. Primaria also focuses on improving communication and collaboration among clinicians, including primary care clinicians, specialists, case managers, social workers, and other team members. For example, physicians who identify a patient with a social need, such as transportation to an appointment, can contact a resource coordinator to work with the patient and arrange transportation. With the pandemic stalling many preventive health screenings, the Primaria Quality Team is redoubling efforts to notify patients who are overdue for preventive care. If patients are unable to make an in-person visit for certain screenings, the ACO sends an at-home screening kit.